Uncategorized
Webinar on Building Resilience for Family Caregivers
In February our Executive Director, Roy Remer, presented a webinar for the Family Caregiver Alliance called Genuine Resilience is Closer (and Easier) Than You May Think. We have posted it below for anyone to access.
In the webinar, Roy talks about how to develop a mindfulness practice in a busy life, ways to use self-compassion when feeling overwhelmed and inadequate, and simple practices for maintaining healthy boundaries. It is an interactive experience that provides tools for developing a greater sense of peace and well-being.
The Power of Setting an Intention
Before leaving bed in the morning, I have been sharing an intention for the day with my wife; and she shares hers. Today I have a lot to accomplish, and my intention is to stay focused and be kind to myself. The intention I set in the morning informs my day in subtle or profound ways depending on the extent to which I keep it in my conscious awareness. It is quite easy to lose contact with the intention and then it is just a nice way to start the day. Ideally, however, intention becomes a bit like focusing on the breath in meditation, in that when I veer too far from my intention, I return my attention to it. Again, and again. I marvel at this aspect of being human; we can move toward growth and change by imagining who we want to be in the world in the present, but also in the future. And, setting an intention can keep our aim true.
I have been thinking about how useful it is to work with intention in the context of caregiving. Whether we care for a loved one or care for a patient, using intention can be extremely supportive. Caregiving offers many rewards, however, it can at times be really challenging; it asks a lot of us. We all need a little support from time to time. Using intention can be a way of coaching oneself to be our best. Not just to provide the best care possible—something we all want—but also to nurture our self in the best way possible. Setting an intention clarifies what is most important. It allows us to step back for a moment and consider how we want to show up before taking on a task or entering into an encounter. Setting an intention can activate meta-awareness, or knowing you are having an experience, as opposed to simply having an experience. Meta-awareness is something we are all capable of activating if we can pause long enough to step back and observe our own actions, attitudes, or emotions. This kind of awareness can help keep us from getting swept away in negative thoughts or behaviors; the stuff that just makes things worse.
When we set an intention for our caregiving experience, we provide our self with a guidepost. Instead of getting lost in the immediacy of challenging circumstances, we can more readily check-in and ask, am I showing up the way I want to show up for this experience. Setting an intention for openness may allow us to meet a family member of a patient who usually triggers us with more understanding or patience. Or, setting an intention for calmness can support us to stay grounded when mom starts getting agitated when she is not understood. Or, an intention to take better care of myself today can help us remember to step outside in the midst of our busy day to simply pause and remember that the trees still bloom after a long cold winter.
Well, it doesn’t hurt to try, right? Consider intention setting a small thought experiment. You can try it now after reading this… take a deep breath, another, then consider what your intention is for how you want to show up for the remainder of the day. Something simple. The most powerful intentions are short and to the point. Perhaps you write it down on a post-it note or commit it to memory. But either way, carry your intention with you and return to it when you need it. See if it helps. I am confident it won’t make things worse. And that is something.
The Challenges of Caregiving
From a recent study conducted by the AARP and the National Alliance for Caregiving,
“…there are more than 43.5 million adults in the United States who have provided unpaid care to an adult or child within the last year. 34.2 million of these Americans provide care to an adult age 50 or older. On average, a family caregiver will spend over 24 hours each week providing care to a loved one, although many report spending over 40 hours per week on caregiving duties.”
Caregiving, in any capacity, can be quite rewarding but it also comes with its own set of challenges. For some, caregiving can be stressful, overwhelming, strenuous and frustrating. Asccare.com lists a number of difficulties for you to pay close attention to, here are a few;
- Depression and isolation
- Sleep deprivation
- Emotional and physical stress
- Lack of privacy
- Being afraid to ask for help
- Financial strain
- Managing time
Coping with any one of these challenges can be trying though many of you face multiple challenges on a daily basis. Thankfully there are mindfulness-based tools and approaches to help you build emotional resilience to maintain delivery of high-quality and compassionate care to your loved ones.
Our Mindful Caregiving Education (MCE) introduces caregivers to mindfulness-based approaches and tools to help build their emotional resilience and work with stress. These approaches help caregivers successfully navigate the unique and challenging situations that can arise in caregiving. Through mindfulness-based education, you can build the skills needed to take on the common challenges of caregiving.
Zen Caregiving Project’s Mindful Family Caregiving, Four-Part Online Series, starting April 7, helps family caregivers find support and community while sharing resilience-building tools to improve the caregiving experience. This online series will help you:
- Increase the capacity to cope with discomfort and suffering
- Create a plan for maintaining self-care
- Establish healthy boundaries in relationships
- Deepen and sustain compassion for self and others
I invite you to take a moment and consider our Mindful Family Caregiving course and see if it fits with your schedule. If you have any questions, feel free to email us at education@zencaregiving.org
The Bathing Ritual at Laguna Honda Hospital
By Alistair Shanks
In a small room on the second floor of a Victorian house in San Francisco, eight people are gathered around a bed, autumn light pale on the faces and walls. A man, dead less than an hour, lies on the bed, head resting on the pillow, grey-white hair brushed in feathery strands, arms at his sides outside the covers, palms down. Except for the greyish pallor of his skin and unnatural stillness of his body, he could be asleep. Next to the bed is a table draped with a gold tablecloth and arranged with flowers, a bell, a candle, and a bowl containing an herbal brew. A volunteer rings the bell and the sound dissolves slowly into the silence of the room.
We are here to perform the “bathing ritual,” a ceremony that allows family, friends, volunteers, and staff to say their goodbyes to those they have loved and cared for. This scene has been repeated countless times over the years as Zen Hospice staff and volunteers have performed this ritual at the now-closed Guest House.
A middle-aged man steps forward, picks up a washcloth from a tray held by a volunteer and dips it in the bowl containing the herbal brew. It is Yerba Santa, translated as “holy herb,” also known as Penny Whistle, a fragrant herb that grows locally and is used by native American peoples for a variety of cleansing rituals. He squeezes it out and approaching the bed, picks up the dead man’s left hand and gently wipes it with the cloth, turning the hand over delicately to cleanse the palm and fingertips. His voice catches in his throat as he murmurs, “Thank you, Dad, for the way you always looked out for me… I love you…” His voice trails off into the stillness of the room.
Zen Caregiving Project volunteers care for people nearing the end of their lives, finding ways to provide companionship, kind attention, and a loving presence during whatever time they have left. As someone weakens and nears death we sit with them silently, offering a simple witnessing presence to their final hours, minutes, and breaths.
Our care does not end at death. For family and friends of a deceased loved one, as well as volunteers and staff, what happens after death, can be just as significant as the care they receive in their last weeks and days. Too often people don’t know what to do in those raw moments after their loved one has died. In many cases, we have lost the traditions and practices for honoring and marking the passing of those we love.
One by one the people in the room take their turn choosing a washcloth, dipping it in the Yerba Santa mixture, squeezing it out, and approaching the bed to cleanse the hands and face of the deceased man. Many do this in silence, some speak words of love and sadness, gratitude. When all have taken their turn we stand in silence until the volunteer rings the bell, sharp and clear in the stillness.
Since its beginning, Zen Hospice Project has offered this simple bathing ritual for deceased residents. It is a way to mutually engage family, friends, volunteers, and staff in a tangible enactment of love and grief. This tender act of cleansing may be the last opportunity family and friends have to touch their loved one.
Despite its long history at the Guest House, this ritual had never been done at Laguna Honda Hospital until October 12, 2019, when Zen Caregiving volunteers, with the support of hospital staff, performed it for 40 friends and family members of a deceased patient. Attendees ranged in age from seven to 79 years of age. Some participated actively, others observed. ZCP volunteer Audrey Meinertzhagen described it as a “force field of urgent love.”
In the institutional setting of a large, public healthcare facility that does not lend itself to intimacy, the enactment of this ritual takes on even greater significance. The true beauty of the bathing ritual lies not in creating a perfect environment, although all efforts are made to create a serene and safe space for its enactment. Its power comes from the careful and loving actions of the community of participants and the opportunity to express deep loss in a tangible way. We at Zen Caregiving Project are excited to be able to offer what the resident’s daughter described as a “loving and compassionate farewell,” to the families of residents who die in our care.
Hospice Myths: 6 Things Hospice Care Isn’t
Hospice care is often misunderstood, which can lead to confusion about what hospice is and is not. We dispel six hospice myths.
Hospice isn’t a place but a type of care.
Hospice care provides the highest quality of life possible during the time your loved one has remaining. Hospice focuses on alleviating pain and other symptoms while addressing emotional and spiritual needs.
Hospice care isn’t something to be feared.
While hospice doesn’t treat the illness, it maximizes the patient’s quality of life in their final months. Hospice addresses the spiritual and emotional needs of the patient while providing comfort at the end of life.
Hospice care isn’t about giving up.
Hospice isn’t about giving up hope but redefining hope by helping patients to restore relationships, find peace, and spend time with their loved ones without aggressive medical intervention that often is painful and intrusive.
Hospice care isn’t just for cancer patients.
Hospice is a special kind of care for anyone living with any serious illness that has been diagnosed with six months or less to live by their doctor or specialist. If a loved one has suffered from a stroke, dementia, ALS, MS, liver disease, heart disease, or other serious illnesses, he or she may benefit from hospice care.
Hospice care isn’t to cure the underlying disease.
The goal of hospice care isn’t to cure the underlying disease; its focus is on symptom management, pain control, and comfort so that the patient can enjoy the highest quality of life possible during the time remaining. Hospice care also provides counseling, practical support, and respite.
Hospice care isn’t always an easy choice.
Family and friends must remember that hospice exists to provide compassionate care for loved ones at the end of their life when it has been determined that there is nothing medically that can be done to reverse or cure the underlying disease. Hospice care focuses on pain alleviation and symptom control and encourages an emphasis on emotional healing and relationships.
Mindful Caregiving Education Explained
We’re pleased to share a short video that explains the key components and benefits of our Mindful Caregiving Education program. We hope you will take a moment to watch the short animated presentation, and share it with anyone who you feel could benefit from learning more about our caregiver courses.
For more information click here https://zencaregiving.org/mindful-caregiving-education-explained/
The Challenge of Maintaining Healthy Boundaries
I have had the privilege of meeting many caregivers in my role of teaching Mindful Caregiver Education courses at Zen Caregiving Project. An issue that comes up, again and again, is the challenge they face of maintaining healthy boundaries. Boundary violations — when someone oversteps the limits of another’s comfort zone — are common in the caregiving experience because they are common in life. Interacting with others regularly means that we will bump up against emotional boundaries. There is really no way around it.
Some examples of boundary violations are:
A daughter caring for her father feels a boundary was crossed when he asks her to clean his house, so he does not have to pay a housekeeper.
A brother feels a boundary is crossed when his caregiving sister won’t let him speak for himself during an appointment.
A nurse feels a patient has crossed a boundary when the patient asks for a personal phone number to call after hours.
In our Mindful Caregiver Education courses, we help people recognize when their boundaries have been crossed and teach them skillful ways of responding to boundary violations. We are not teaching how to eliminate boundary issues. In fact, this really is not possible. However, caregivers can learn to respond skillfully, so their response does not worsen the situation. Boundary issues are complex, and learning to respond skillfully takes practice.
Whether or not we experience a boundary violation can depend upon how well-resourced we are feeling on any particular day. Sleep, nutrition, relationships, and stress can all influence how we handle boundary issues. Emotional boundaries are fluid and can change from day-to-day.
And, boundary issues go both ways. Often caregivers experience the recipient of their care overstepping a boundary. Yet, if a caregiver is not paying attention, they too can violate boundaries.
So, recognizing boundary issues and learning healthy ways of coping with them is really important for the long-term well-being of both caregiver and care-recipient.
Mindfulness is a key tool in recognizing and working with boundary issues. Sometimes we may not realize that our boundaries have been violated; we just feel that something is not right. When we lack clarity around what is happening, we can react unskillfully, and things just get worse. In this scenario, we can use mindfulness to deepen an awareness of the body and physical sensations. The body does not lie; it can know that something is not right even before we understand what is really happening.
Learning to pay attention to the body through mindfulness practice can also help us pause before reacting unskillfully. One of my favorite pieces of wisdom comes from the writer/philosopher Victor Frankl who wrote, “Between stimulus and response, there is a space. In that space is our power to choose our response. In our response lies our growth and freedom.” When we are paying attention to our own body and mind, we can actually choose our response in any given situation. We can respond to boundary issues in a way that clarifies our own needs while conveying clearly that the relationship matters.
Conveying a clear boundary to a loved one, or to someone we are caring for, can be an act of compassion. It conveys that we are at once, committed to caregiving, and committed taking care of oneself. These commitments are not separate. Finding ways to take care of oneself actually supports better caregiving. Better caregiving is what we are encouraging at Zen Caregiving Project. Let us know how we can support you.
Dying Days at the Guest House
By Celeyce Matthews
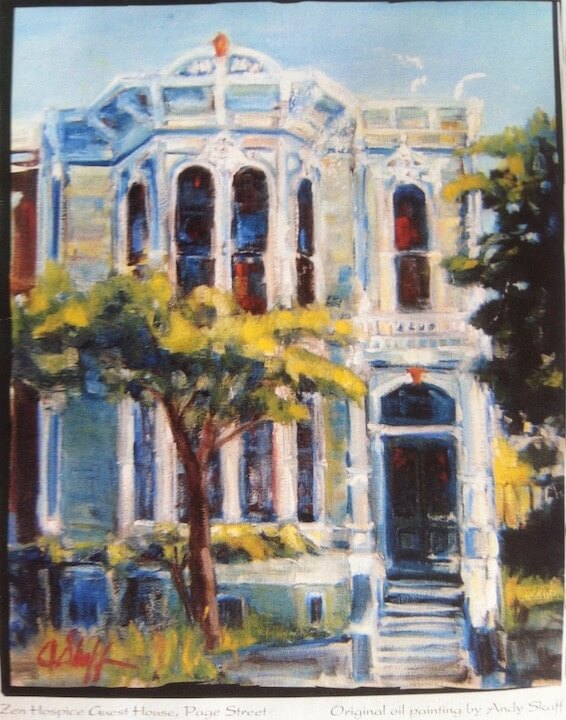
Although I love my new job as a neonatal intensive care nurse, I miss my work in hospice on a daily basis. Before I was a NICU nurse, I was a certified hospice and palliative care nurse assistant at Zen Hospice Project’s now-defunct Guest House. The Guest House was a six-bed hospice residence in an iconic Victorian home in San Francisco, caring for people at the end of life. In its own last year of life, the Guest House had fewer and fewer residents due to complex political and financial issues. While it was extremely painful and frustrating to watch that beautiful place slowly die after serving as a graceful home of living and dying for more than 30 years, its decline also afforded some exceptional experiences that I will forever be grateful for. And frankly wonder if will ever be matched in meaning and beauty.
Some weeks that last year we only had a couple of residents at the Guest House, and in my 12-hour shifts, I was able to spend significant time with people in their final days and minutes and be with them as they took their last breath. While there are some similarities between the NICU and hospice, the beginnings and ends of life, the intense clinical pace of the NICU does not allow for the meaningfulness of the work to register as keenly as the spaciousness of the Guest House allowed for, especially in its final year. The deep sense of peace mixed with the shared experiences of love, anguish, sadness, suffering, beauty, and gratitude as I cared for people letting go of life was profound. Real and raw, in the midst of truth and complexity, love, and pain, I found passionate equanimity; I found a home.
“Alan” was chatty the first day I met him. Jittery in his movements, his emaciated limbs shaking in his grand, arching gestures, he told me stories of growing up gay and black in an area of the country not welcoming of these identities. He rarely paused between his words, so incessant was his need to talk, to speak his life as it was slipping away. In the next days, he became silent but insisted on sitting upright on the side of his bed. His long, ethereal body precariously balanced, wavering as if just about to collapse, his eyes half-closed, teetering on the edge. He would sit like this all day, only willing to get in bed to be gently bathed. He also wanted basketball games to be continually on his television. Concerned about him falling, and because I had the time with only one other resident in the house who was being looked after by the other caregiver, I spent hours just sitting with Alan in his room. He seemed to be hovering in a liminal space, not fully here but not gone, as the sounds of a basketball game, the sounds of life, quietly played on in the otherwise quiet room.
As I sat with him, I became attuned to him, knowing when he was about to reach for a tissue to wipe his leaking mouth and handing it to him just as he lifted his hand. Occasionally he would become aware of me and turn toward me and say, “Oh, you’re still here.” “Yes,” I’d say, “Is that ok with you?” “Yeah, thank you,” he would sometimes say, sometimes only finding the energy to nod slowly. In that quiet drama of stillness and basketball and afternoon light and Alan’s struggle to stay upright wavering between life and death, I felt a deep human kinship and connection between us. Our differing backgrounds and current circumstances dissolved in the reality of approaching death. At the rawest and most stripped-down level that the end of life brings, we were just two humans sitting together on the precipice.
And the caring – caring about this man I didn’t really know, caring for his body in ways that he could no longer do for himself – caregiving felt like a sacred thing, one that nourished me deeply. Bathing the dying, changing their briefs, feeding them, receiving their life stories, holding their hands felt like an incredible privilege to me. In a way, I needed it as much as they did. I miss this every single day.
The last time I saw Alan, he had finally consented to lying safely in his bed, no longer able to sit upright on his own at all. It was a busier day, and I didn’t have as much time to sit with him. When I came to say goodbye and tell him that I was going out of town for a week, we both clearly understand that this was goodbye forever. He started to cry and reached for me. I think this was the moment that the closeness of his death became even more starkly clear to him; the chronicling of the lasts and the losses getting close to the bottom of the page. He thanked me, and I could again feel the care and connection between two humans flow between us. I hugged him and quietly beamed my love and gratitude to him, marveling at how loss, love, and sadness are woven into the fabric of life. I was sorry to not be there for his death.
To not flee from these realities of humanity, of life, love, and loss, to stay with them unflinchingly was my job, but more importantly, it is my calling.
Being in the highly clinical and yet heart-centered world of the NICU, these aspects of care can feel sometimes eclipsed by the intense technology and the often breakneck pace. But the moments of placing a sick premature baby on his mother’s bare breast for the first time, or teaching a new father how to change the diapers of his 3 pound baby, or holding and bottle feeding a cute growing baby, I feel the gifts of caregiving. The clinical demands of the NICU are not what I ever wanted to be involved in, but those tiny, fragile babies seduced me.
And so here I am, at the other end of life, the beginning. One day I will have to return to hospice, I truly do miss it daily. Although I may never be gifted with the spaciousness of time to just be humans together living and dying, and engage in slow, gentle, mindful care as I was lucky to do in the dying days of the Zen Hospice Project’s Guest House.
10 Tips for Caregivers Over the Holidays
The holidays can be a joyous but stressful time (but it doesn’t have to be stressful). We offer 10 tips for caregivers to take care of themselves over the holidays.
1. Practice self-love
While the holidays can be stressful, it’s essential to take care of your physical and mental health. Keeping yourself healthy produces positive outcomes and improves the quality of care for those who depend on you.
2. Keep it simple
Remember, you have only so much energy and so many resources, don’t expend them at the expense of your own health. Keeping things simple and stress-free will save energy and your mental health.
3. No-stress meals
It’s ok to go out for meals or order in. The point is to enjoy the time together with those you love. If the time spent preparing a meal is more stressful than it’s worth, skip it.
4. Start a new tradition
Sometimes getting out and about isn’t possible due to personal responsibilities and time constraints. Invite people over to decorate, watch holiday movies at home, make yourself your favorite treat. You can develop new traditions that fit your life.
5. You can ask for help
Ask your friends and family to help with cleaning or groceries, shoveling the walk, tidying up. If resources allow, you can also order the things you need online or hire someone to help you.
6. Shop online
With so much going on, it’s challenging to find time to shop for gifts. Don’t be afraid to shop online for gifts and groceries, it’s a great time saver and keeps things relatively stress-free.
7. Brush off negativity
It’s the time for connecting with loved ones but also a time to keep our differences in check. Negative comments may come and go but don’t own them, brush them aside. Enjoy the time with those you love.
8. Let go of perfection
Don’t let perfect be the enemy of the good. You have limited resources and limited bandwidth, work with what you have but leave perfection behind. The point is to enjoy the season.
9. Connect with caregivers
If you haven’t already, connect with caregivers in your community or find online communities to share your thoughts and gather tips. This is a great time to lean on these communities as you process the holidays.
10. Go with the flow
Take things as they come, there’s little need to stress about things that are beyond your control. You’ll feel much better physically and emotionally, but let go of the little things and allow yourself to enjoy the company of those you love.
Zen Caregiving Project New Volunteer Training Update
“Working with the dying, you are constantly reminded of what matters: love, kindness, generosity, and our interconnectedness.” ~ Roshi Joan Halifax
Zen Caregiving Project will soon be taking applications for our Spring 2020 New Volunteer Training, to be held in April. The core training — an intensive 40 hours over ten days — is not oriented towards acquiring skills, so much as asking participants to examine and reflect on their own histories of loss and grief. By exploring our relationship to these issues, we become familiar with our own stories of suffering, enabling us to become more comfortable with the suffering of others. In other words, by becoming intimate with our own losses, our fears, and insecurities, we are more fully able to connect to the loss of others. We learn to connect through our shared vulnerability. This reflects the fundamental Buddhist teaching of interdependence and the Zen Caregiving philosophy of mutuality of service.
Please note that our open enrollment period runs until February 28th, and notification of the status of your application will not be sent out until mid-March. Applicants are required to attend all training sessions, including the Ongoing Sessions. We also ask participants to commit to a full year of service, volunteering one five hour shift per week on a regular schedule.
The application form for the New Volunteer Training will be live and accessible here on Monday, December 16th.
Zen Care Giving Project Spring 2020 New Volunteer Training Dates
Core Training
Wednesday & Thursday, April 15 & 16 (Evening Sessions), 5:45 PM – 10:00 PM
Saturdays & Sundays, April 18, 19, 25, & 26 (All Day), 8:30 AM – 5:30 PM
Ongoing Training (Third Tuesday Evening of the month)
Tuesday, May 19th, 7 PM – 9 PM
Tuesday, June 16th, 7 PM – 9 PM
Tuesday, July 21st, 7 PM – 9 PM
Tuesday, August 18th, 7 PM – 9 PM
Tuesday, September 15th, 7 PM – 9 PM